
Leaders gain a more efficient, reliable operation. Providers gain time back. Your organization gains a workflow engine that’s repeatable, scalable, and built to support expansion.
AI agents complete work in parallel across multiple departments, helping cut administrative time, lower per-provider support costs, and keep your organization’s resources focused where they matter.

AI-backed standardization brings stability to high-volume operations and simplifies onboarding during expansions or acquisitions.
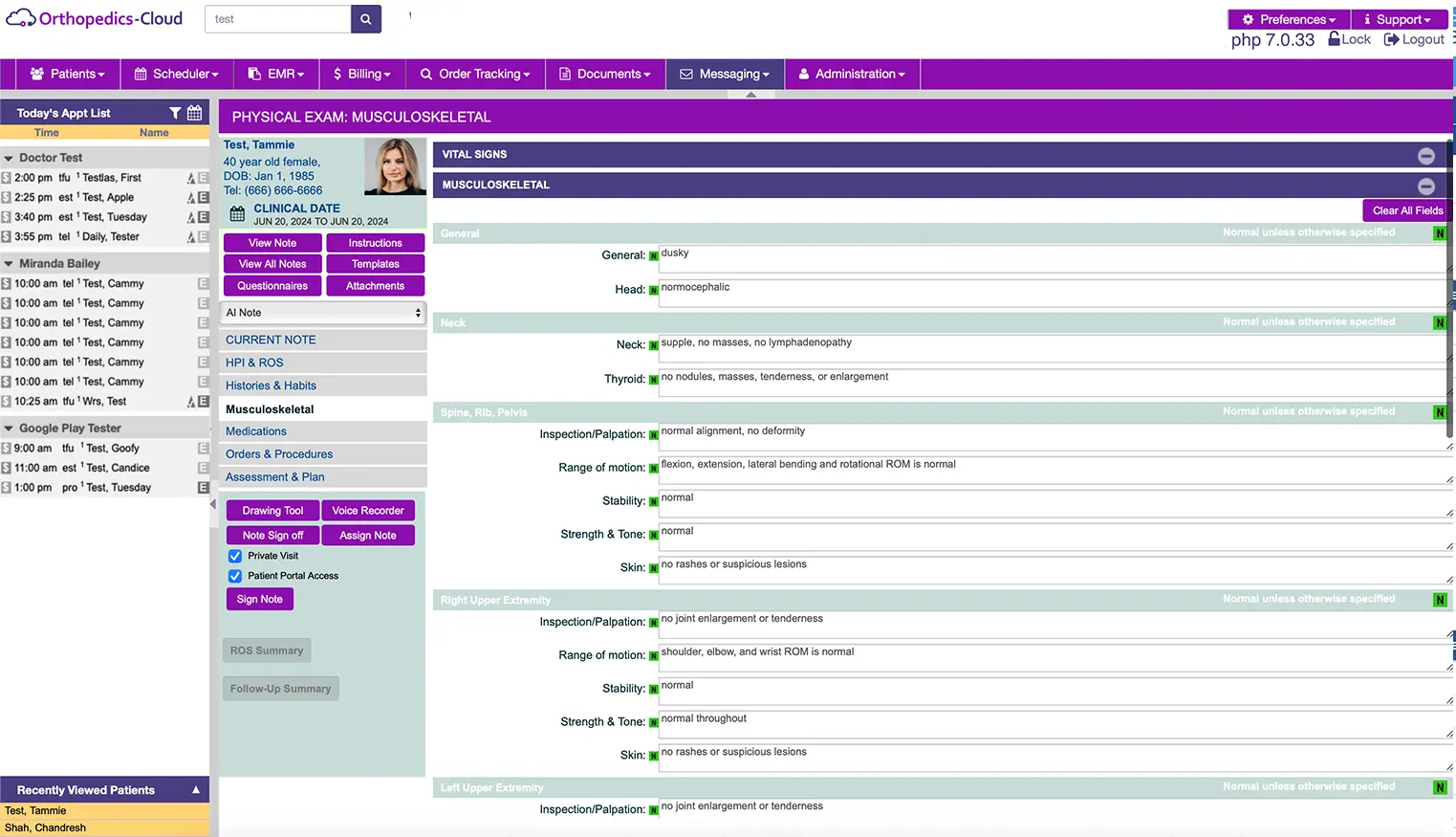
AI-generated encounter notes
Auto-coded visits aligned with payer rules
Automated claim creation
Real-time alerts for missing or incomplete items
The result is a shorter workday for clinicians and a sharper throughput curve for the organization.
AI minimizes the costly steps that slow down revenue:
Eligibility and benefits checks run automatically
Codes are validated before claims are submitted
Claim creation happens as part of the documentation process
Payer-specific rules are applied behind the scenes
Intelligent RCM strengthens cash flow and reduces the need for large billing teams as your practice expands.
Lower administrative cost per provider
Better forecasting around staffing needs
Greater resilience during rapid expansion
The ability to redirect resources to strategic initiatives
